Genauer Blick in die Lunge
Röntgen und Fluoreszenz zeigen, wie sich Medikamente in der Lunge ausbreiten
2020-01-31 – Nachrichten aus dem Physik-Department
Lungenkrankheiten wie die chronische obstruktive Lungenkrankheit (COPD), Asthma oder Infektionen lassen sich seit langem effizient mit Medikamenten behandeln, die von Patientinnen und Patienten eingeatmet werden. In Zukunft sollen weitere Arzneimittel auf diese Weise verabreicht werden – zum Beispiel Mittel gegen Krebs, bei denen der Wirkstoff in Nanopartikeln gebunden ist. “Solche Nanopartikel-basierten Medikamente haben zahlreiche Vorteile,” erklärt Otmar Schmid, Arbeitsgruppenleiter am Institut für Lungenbiologie des Helmholtz Zentrums München. “Zum Beispiel werden die Wirkstoffe nicht so leicht enzymatisch abgebaut, weil sie in dem Nanopartikel eingebettet sind. Außerdem lassen sich die Nanopartikel gezielt zu den erkrankten Zellen lenken, wenn man an ihnen Liganden befestigt, die an diese Zellen andocken.” Damit könnte die Wirkung des Arzneimittels besser auf das erkrankte Gewebe fokussiert werden, was die Nebenwirkungen deutlich reduzieren würde.
Forschende der Arbeitsgruppe von Otmar Schmid haben nun zusammen mit Kolleginnen und Kollegen am Physik-Department und der Munich School of BioEngnineering (MSB) der Technischen Universität München (TUM) eine Kombination von bildgebenden Verfahren vorgestellt, mit denen sich im Detail zeigen lässt, wie die Medikamentenverteilung in der Lunge einer Maus davon abhängt, auf welche Weise die Medikamente verabreicht worden sind. Die Ergebnisse solcher Untersuchungen sollen wichtige Erkenntnisse für die Entwicklung von Lungen-Medikamenten für Menschen liefern.
Lunge am Beschleuniger gefilmt
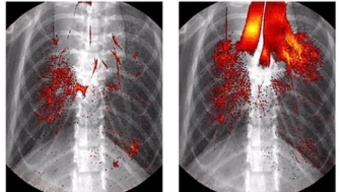
Die Forschenden der TUM haben dabei zwei Verfahren beigetragen, die Röntgenlicht nutzen. Mit einem davon konnten sie einen Film erstellen, der zeigt, wie sich bei einer Maus eingeatmete Medikamente mit der Zeit von der Luftröhre aus in der Lunge ausbreiten. Mit dem zweiten haben sie dreidimensionale Bilder der gesamten Lunge erzeugt. Für die Untersuchung verabreichten sie statt eines echten Medikaments eine Lösung mit Nanopartikeln, die aber keinen Wirkstoff enthielten. Dieser mischten sie zudem ein iodhaltiges medizinisches Kontrastmittel bei, das in Röntgenbildern deutlich sichtbar wird.
Den Film stellten die Forschenden aus Röntgenbildern der Mauslunge zusammen, die sie immer zum gleichen Zeitpunkt im Atemzyklus aufgenommen hatten. “Wir haben bei den Aufnahmen den Propagationseffekt der Röntgenstrahlen ausgenutzt und konnten so auch die Gewebestrukturen der Lunge deutlich sichtbar machen,” erklärt Regine Gradl, die die Messungen im Rahmen ihrer Doktorarbeit am Lehrstuhl für Biomedizinische Physik der TUM durchgeführt hat. “In gewöhnlichen Röntgenbildern hätte man fast nur den Brustkorb und das mit Iod markierte Kontrastmittel gesehen”. Beim Propagationseffekt nutzt man aus, dass die Röntgenstrahlen auf ihrem Weg durch das Untersuchungsobjekt zum Teil geringfügig abgelenkt werden und so verschiedene Strahlen hinter dem Objekt interferieren können. Dank dieser Interferenzen werden im Röntgenbild zusätzliche Details erkennbar. Dazu gehören insbesondere Grenzflächen von Weichgewebe – zum Beispiel zwischen Luft und Lungengewebe.
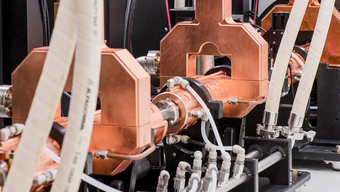
Bis vor kurzem waren solche Untersuchungen nur an Synchrotronlichtquellen möglich, aufwendigen Beschleunigeranlagen mit oftmals mehreren hundert Metern Umfang, denn nur diese lieferten Röntgenlicht, das intensiv und für die Interferenz hinreichend kohärent ist. Seit wenigen Jahren erzeugt mit der Munich Compact Light Source (MuCLS) erstmals eine Anlage, die in ein Labor üblicher Größe passt, Licht mit diesen Eigenschaften. Dieses weltweit einzigartige Mini-Synchrotron wird im Hauptgebäude der MSB in Garching betrieben und ist nur rund 5 mal 3 mal 2 Meter groß. Es ermöglicht Forscherinnen und Forschern, umfangreiche Untersuchungen mit intensivem, kohärenterem Röntgenlicht zeitlich flexibel durchzuführen. “An Synchrotronlichtquellen ist die Nachfrage nach Messzeit sehr groß, so dass Forschende ihre Experimente sehr lang im Voraus planen und in wenigen Tagen durchführen müssen”, betont Gradl. An einer üblichen Laborröntgenquelle wären die Untersuchungen in dieser Form hingegen gar nicht möglich gewesen.
Fluoreszenz zeigt genaue Verteilung

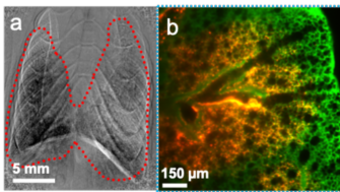
Die Wissenschaftlerinnen und Wissenschaftler am Helmholtz Zentrum München konnten anschließend mit Hilfe von Fluoreszenz-Verfahren an der explantierten Lunge zeigen, wie sich die eingeatmeten Partikel auf die einzelnen Zellen der Lunge verteilt hatten. Für diese Untersuchung waren fluoreszierende Nanopartikel verwendet worden. Werden diese mit Licht angeregt, leuchten sie und zeigen so, wo sich die Lösung in der Lunge befindet. Besonders präzise Ergebnisse konnten die Forschenden dabei mit der sogenannten Lichtblattfluoreszenzmikroskopie (englisch: Lightsheet Fluorescence Microscopy, LSFM) erzielen, bei der jeweils nur eine sehr dünne Schicht der Probe beleuchtet wird, dadurch aber Schicht-für-Schicht ein sehr genaues dreidimensionales Gesamtbild der Lunge und darin lokalisierten Nanopartikel aufgenommen wird.
Einzigartige Kombination
“Mit der Kombination von Röntgen- und Fluoreszenzverfahren können wir erstmals sowohl die Dynamik als auch die Endverteilung) der Verabreichung von Lungenmedikamenten beobachten,” betont Schmid. Damit sollte es in Zukunft zum Beispiel möglich werden, zu bestimmen, wie genau nanopartikelbasierte Medikamente das Zielgewebe erreichen. Aber auch schon die ersten Versuche haben wichtige Erkenntnisse geliefert. Die Forschenden haben hier zwei Methoden verglichen, mit denen Medikamente in präklinischen Studien in die Lunge verabreicht werden: die Inhalation von Tröpfchen und die Instillation von Flüssigkeiten, bei der die Lösung über einen Tubus durch die Trachea in die Lunge injiziert wird. Die Forschenden konnten dabei zeigen, wie es möglich ist, dass sich die instillierte Flüssigkeit bis in die feinsten Verästelungen der Lunge verteilt. “Sie sammelt sich zuerst in den oberen Atemwegen, bis sie diese blockiert, und dann beim nächsten Atemzug als Spray in der ganzen Lunge verteilt wird”, erklärt Schmid. “Anders als bei der Inhalation erreicht sie dabei aber nicht die tiefsten Bereiche der Lunge”.
Veröffentlichung
Verwandte Meldungen
- Interdisziplinäres Studium und sehr gute Berufsaussichten – 2019-11-16
- Modelle des Lebens – 2019-01-17
- Histologie in 3D – 2018-02-22
- Mini-Teilchenbeschleuniger spart Kontrastmittel – 2017-02-27
- Neue hochmoderne Röntgenquelle auf kleinem Raum – 2015-10-29